Polymerase Chain Reaction (PCR) is a standard laboratory technique used to amplify a specific sequence of DNA many times over. This technique has become an important tool in clinical laboratories for the detection of infectious pathogens that do not grow in conventional culture media.1 PCR-based methods are powerful techniques2; with the ability to detect a single molecule of DNA, disease can be detected at extremely low levels. Such sensitivity, however, makes PCR highly susceptible to cross-contamination, particularly from exogenous DNA sources. The most common sources of contamination include sample to sample transfer and amplicon carryover.3
The consequences of contamination can be severe and include erroneous results, extensive investigation to identify the source of contamination, cleanup leading to laboratory downtime and delays, as well as loss of credibility. Implementation of safeguards and strict adherence to robust protocols such as those summarized below is often sufficient to ensure that cross-contamination in the molecular laboratory is a rare event.
Laboratory Construction
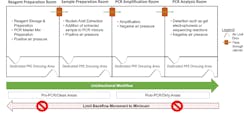
The layout for a molecular laboratory should be designed to allow for areas dedicated for sample and reagent preparation and for amplification reaction and detection activities (e.g., agarose gel electrophoresis, when necessary).4 Ideally, a molecular laboratory would be designed with three or four separate rooms, dependent on the PCR method used.5 At a minimum, it is recommended to have two separate rooms defined as a pre-PCR/clean room where sample preparation steps such as DNA/RNA extraction and PCR preparation occur, and a post-PCR/dirty room where PCR reactions and other post-PCR analyses are performed.5 In scenarios where space does not permit dedicated rooms, separate benches should be identified for pre-PCR activities (reagent preparation, sample preparation) and post-PCR activities (PCR amplification, PCR analysis). As an additional control when all PCR steps are performed in the same room, timetables can be established where pre-PCR and post-PCR steps are performed at different times of the day.4
Reagent Preparation room.5 The cleanest of all spaces used for PCR, this room is dedicated to activities such as preparation and aliquoting of reagent stocks. In addition, reaction mixes may also be prepared here, excluding the addition of the extracted nucleic acids from the clinical sample. To reduce the possibility of contamination, extracted DNA/RNA and/or PCR products should never be present in the reagent preparation room.
Sample preparation room.5 Because it is important to keep PCR products away from where clinical sample extraction occurs, this room is generally split into two areas: one dedicated to DNA and/or RNA extraction activities and one dedicated to nucleic acid addition to the PCR reaction mixtures. The reverse transcriptase step of reverse transcription (RT)-PCR is performed in this room, as well as the addition of DNA or cDNA, and positive controls to the PCR reaction mixture. Ideally isolated nucleic acids are added to PCR reaction mixes in a laminar flow hood.
PCR amplification room.5 PCR instruments (i.e., thermocyclers) used for amplification steps are kept in this room. Additional analysis is not required for real time PCR, and tubes containing RT-PCR products should never be opened.
Post-PCR analysis.5 When agarose gel electrophoresis is required, it should occur in a dedicated room/area as it will be contaminated with amplicons from the PCR reaction. A laminar flow hood is recommended for any steps requiring the opening of tubes containing amplicons. To control for contamination, it is also critical that personnel performing post-PCR analysis not return to pre-PCR work areas in the same day.
Engineering Controls
Air flow.6 The reagent preparation room should have positive air pressure to keep contaminants out. In contrast, the post-PCR analysis room should be under negative air pressure to keep amplicon contaminants in. When possible, the air handlers for the different PCR areas should be connected to separate air ducts, with each leading to a separate location for exhaust.
Air lock doors. Ideally, a vestibule provides the main access point to the clean room and is constructed with two or more doors. The interlock function allows only one door to be open at a time. By preventing both doors form being open simultaneously, air and airborne particulates are unable to enter or exit the airlock, thus reducing the opportunity for cross-contamination.
Laboratory Operation
UnidirectionaI.5 All steps should occur sequentially moving from clean room to dirty room. For example, PCR protocols should begin in the reagent preparation room, move to the sample preparation room, and end in the PCR amplification or post-PCR analysis room. This helps to ensure reduce the risk of contamination by keeping clean areas free of amplicons.
Pass through air locks. Use of pass-through cabinets can facilitate a unidirectional workflow. These boxes are designed to maintain complete environmental separation between work areas and minimize cross contamination.
Dedicated Personnel.5 Laboratory personnel dedicated to either clean room activities or dirty room activities is recommended. Clean lab coats and gloves should be worn when performing PCR; gloves should be changed frequently. In the event that laboratory personnel need to move from a dirty room back to a clean room, all personal protective equipment (PPE) should be changed, and hands washed.
Dedicated consumables and equipment.5 The availability of dedicated storage (e.g., freezer, fridge) in each room prevents movement of reagents and samples between dedicated areas, thereby minimizing the potential for contamination. In addition, consumables (e.g., lab coats, gloves, goggles, disposable shoe covers, etc.) and equipment (e.g., pipettes, centrifuges, pipette tips, etc.) should never be brought from dirty rooms back into clean rooms.
Aerosol-resistant pipettes. Sample to sample contamination can occur due to aerosols. Use of barrier tips prevents liquids and aerosols from contacting the pipette.
Pipetting techniques. Use of proper pipetting technique can also prevent contamination. This includes ensuring the pipette tip is securely seated on the pipette and aspirating at a vertical 90° angle with consistent smooth speed and pressure. When dispensing liquid, the pipette should be held at a 45° angle with the tip of the pipette touching the side of the receptacle to minimize splashing.
No template control (NTC).7 NTCs consist of all reagents added during preparation of the PCR reaction mixture but uses water instead of the extracted sample. Including an NTC in PCR amplification reactions allows for the identification of contamination in samples, reagents, and/or the lab environment.
Cleaning/decontamination techniques
Surface and Equipment.8 Following appropriate cleaning and decontamination techniques both before and after PCR reduces the potential for contamination of the PCR reaction. Frequent cleaning of work areas with freshly made 10-15% sodium hypochlorite solution (bleach) followed by rinsing with 70% ethanol or cleaning with commercially available DNA-destroying decontamination products is recommended. Alternatively, cleaning of work surfaces and equipment with 70% ethanol followed by irradiation with UV light can also be done; irradiation is critical as ethanol only precipitates but does not remove DNA.
UV irradiation.9 This technique induces thymidine dimer formation in the DNA rendering it unusable as a template for further amplification. Use of UV irradiation is recommended for laminar flow hoods for at least 30 minutes prior to use, followed by cleaning with 70% ethanol.
Additional Considerations
Quality Monitoring Statistics10 As mentioned, the greatest risk source of contamination for PCR-based tests is from exogenous DNA. Laboratories must have clearly written procedures in place to monitor for the presence of false-positive results. This can include implementation of wipe or swipe tests on a defined schedule, positivity rate monitoring by reviewing summary statistics at the local and regional level, and investigations of physician inquiries.
Wipe or swipe tests involve dampening of a sterile swab in sterile saline and wiping potentially contaminated surfaces of a laboratory (e.g., benches, pipettes, handles of fridge/freezer, centrifuges, etc.). These swabs are then processed and tested in manner similar to patient samples. A positive result from a wipe test is indicative of environmental contamination.
Contamination from Serology Testing11 In some scenarios, diagnosis of an infectious disease such as Hepatitis C (HCV) or Human Immunodeficiency Virus (HIV) begins by screening for anti-HCV or anti-HIV antibodies. If antibodies are detected in a sample, further testing a PCR-based method is required for confirmation. When the same sample used for serology testing is also used for nucleic acid testing the potential exists for increased risk of cross-contamination, dependent on the design of the laboratory instruments used for serology testing. For example, instruments using a washable sample probe pose a slightly increased risk for cross-contamination versus instruments that utilize a disposable tip. As a mitigation, it has been suggested that low level RNA results from samples previously tested on a serology instrument with a washable probe be rejected and a new sample requested for repeat PCR analysis. Alternatively for samples screened on an instrument using disposable tips, there may be no need for a separate tube for confirmatory PCR testing.
Conclusion
The safeguards and operational recommendations summarized above serve to prevent contamination of molecular diagnostic tests and subsequent impact to diagnostic and treatment decisions. In many scenarios, molecular testing plays a major role in the management of patients, thus prevention of contamination must be a priority in clinical molecular laboratories.
References
- Aslanzaden J. Preventing PCR amplification carryover contamination in a clinical laboratory. Ann Clin Lab Sci. 2004;34(4):389-396.
- Hu Y. Regulatory concern of polymerase chain reaction (PCR) carryover contamination. In: Samadikuchaksaraei, A, ed. Polymerase Chain Reaction for Biomedical Applications. IntechOpen, 2016:57-68. doi: 10.5772/66294.
- Huggett J, Benes V, Bustin S, et al. Cautionary note on contamination of reagents used for molecular detection of SARS-CoV-2. Clin Chem. 2020;66(11):1369-1372. doi: 10.1093/clinchem/hvaa214.
- Mifflin TE. Setting up a PCR laboratory. CSH Protoc. 2007; pdb.top14.
- Standards Unit, National Health Service, Public Health England. UK Standards for Microbiology Investigations: Good practice when performing molecular amplification assays. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/682533/Q4i5.pdf. Updated February 19, 2018. Accessed March 20, 2022.
- Aysal A, Pehlivanoğlu B, Ekmekci S, Gündoğdu B. How to set up a molecular pathology lab: a guide for pathologists. Turk Patoloji Derg. 2020;36(3):179-187. doi: 10.5146/tjpath.2020.01488.
- Viana RV, Wallis CL. Good Clinical Laboratory Practice (GCLP) for Molecular Based Tests Used in Diagnostic Laboratories. In: Akyar I, ed. Wide Spectra of Quality Control. InTech, 2011: 29-52.
- Prince AM, Andrus L. PCR: how to kill unwanted DNA. Biotechniques. 1992;23(3):358-360.
- Ou CY, Moore JL, Schochetman G. Use of UV irradiation to reduce false positivity in polymerase chain reaction. Biotechniques. 1991;10:442-446.
- Wallace P, McCulloch E. Quality Assurance in the Clinical Virology Laboratory. Encyclopedia of Virology. 2021;64-81. DOI:10.1016/B978-0-12-814515-9.00132-6.
- Rondahl E, Gruber M, Joelsson S, et al. The risk of HCV contamination in serology screening instruments with a fixed needle for sample transfer. J Clin Virol. 2014;60:172-173.
Jeanne Rhea-McManus, PhD, MBA, DABCC, NRCC has been with Siemens Healthineers for 7 years, previously as a Medical Officer and currently as the Senior Director of Medical Science Information and Communication.